Understanding the Bilateral Hysterectomy Procedure: A Complete Guide to Your Women's Health

In the realm of women's healthcare, advancements in surgical techniques have significantly improved outcomes for various gynecological conditions. Among these, the bilateral hysterectomy procedure stands out as a definitive treatment option for a range of health concerns affecting the uterus. This comprehensive guide aims to educate women and prospective patients about this procedure, its indications, the surgical process, post-operative care, and the importance of consulting highly skilled obstetricians & gynecologists like Dr. Seckin for personalized, expert care.
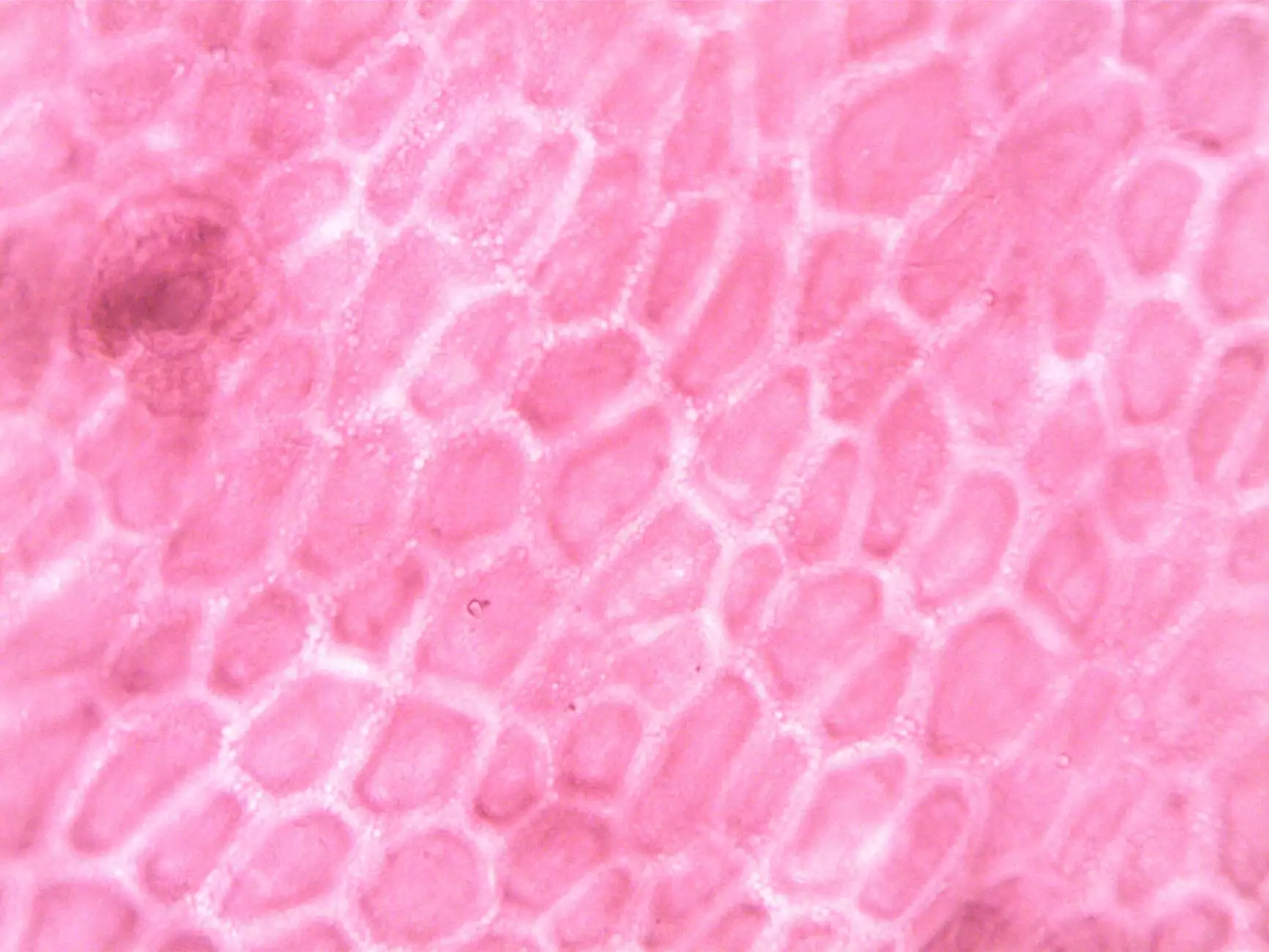
What is a Bilateral Hysterectomy?
A bilateral hysterectomy is a surgical procedure involving the complete removal of the uterus and cervix. The term “bilateral” indicates that both sides of the reproductive system—primarily the uterus and cervix—are excised in a single surgical operation. This procedure may be performed through various surgical approaches, including abdominal, vaginal, or minimally invasive techniques like laparoscopy or robotic surgery, depending on the patient's condition and the surgeon's expertise.
Why Consider a Bilateral Hysterectomy?
The decision to undergo a bilateral hysterectomy procedure is typically made after evaluating significant health issues. Common indications include:
- Uterine fibroids causing severe symptoms such as heavy bleeding, pelvic pain, or pressure
- Endometriosis with refractory pain
- Chronic abnormal uterine bleeding unresponsive to conservative treatments
- Uterine prolapse leading to discomfort or functional impairment
- Persistent or recurrent pelvic tumors or cysts
- Cancer of the uterus, cervix, or endometrial hyperplasia with malignant potential
- Other significant gynecological issues impacting quality of life
Understanding the Surgical Techniques of Bilateral Hysterectomy
The bilateral hysterectomy procedure can be performed via different surgical approaches:
Abdominal Hysterectomy
This traditional method involves an incision in the lower abdomen to access and remove the uterus. It offers direct visualization and is often used for larger uteri or complex cases. Recovery time typically spans 4-6 weeks.
Vaginal Hysterectomy
Performed through an incision inside the vagina, this approach avoids abdominal incisions, leading to less postoperative pain, shorter hospital stays, and quicker recovery. Suitable for women with uterine prolapse or smaller uteri.
Laparoscopic or Robotic-Assisted Hysterectomy
Modern minimally invasive methods utilize small incisions, cameras, and specialized instruments. Robotic assistance enhances precision, reduces blood loss, and accelerates recovery. This technique is increasingly preferred among leading specialists like Dr. Seckin for complex cases.
The Step-by-Step Process of a Typical Bilateral Hysterectomy
A bilateral hysterectomy procedure involves meticulous planning and execution. Here’s what patients can expect:
- Preoperative Evaluation: Comprehensive assessment including imaging, blood tests, and counseling about risks, benefits, and recovery process.
- Anesthesia: General anesthesia to ensure patient comfort and safety throughout the surgery.
- Surgical Approach: Depending on the chosen technique, the surgeon makes the appropriate incisions.
- Isolation of Uterus and Removal: Carefully ligate blood vessels, detach the uterus from surrounding tissues, and remove it entirely.
- Closure and Recovery: Suturing of incisions, ensuring hemostasis, and appropriately managing postoperative pain and care.
Recovery and Post-Operative Care Following a Bilateral Hysterectomy
Postoperative recovery is a critical phase that determines long-term success and well-being. Patients can expect:
- Hospital Stay: Usually 1-3 days, depending on the surgical approach and individual health status.
- Pain Management: Effective pain relief with medications prescribed by the healthcare team.
- Activity Restrictions: Limited strenuous activity for several weeks, with gradual resumption guided by the surgeon.
- Follow-Up Appointments: Regular check-ups to monitor healing and address any concerns.
Potential Risks and Complications of the Bilateral Hysterectomy Procedure
While a bilateral hysterectomy is generally safe, understanding possible risks helps in making informed decisions:
- Bleeding or hemorrhage
- An infection at the surgical site
- Injury to surrounding organs such as bladder or bowel
- Adverse reactions to anesthesia
- Ovarian failure if ovaries are removed, leading to menopausal symptoms
- Formation of adhesions or scar tissue, potentially causing pelvic pain
Choosing the Right Specialist for Your Surgical Needs
Deciding to undergo a bilateral hysterectomy is a major decision impacting your health and life quality. It is paramount to select a surgeon with extensive experience in minimally invasive gynecological surgeries, exceptional surgical skills, and compassionate patient care. Dr. Seckin, renowned in the field of Doctors, Health & Medical, Obstetricians & Gynecologists, offers cutting-edge surgical expertise, personalized treatment plans, and empathetic support throughout your journey.
When choosing your healthcare provider, consider:
- Experience with various hysterectomy techniques
- Positive patient reviews and testimonials
- Availability of advanced surgical technology
- Focus on minimally invasive options for faster recovery
- Comprehensive preoperative and postoperative care
The Future of Women's Gynecological Surgery and Patient Empowerment
The field of gynecology is continuously evolving, with innovations like robotic surgeries, advanced diagnostics, and personalized medicine enhancing patient outcomes. Empowering women with accurate information about procedures like the bilateral hysterectomy procedure helps them make informed choices aligned with their health goals. Education, technological advancements, and compassionate care foster a positive experience and improve quality of life.
In Conclusion: Your Path to Better Health Starts Here
The decision to undergo a bilateral hysterectomy procedure is a deeply personal one, influenced by various medical and emotional factors. Rest assured, with expert surgical teams led by dedicated specialists such as Dr. Seckin, you can expect exceptional care, comprehensive education, and compassionate support throughout your healing journey. Your health and well-being are worth the investment, and modern surgical options provide safe, effective solutions for complex gynecological conditions.
Take proactive steps today by consulting experienced obstetricians & gynecologists who prioritize your health, comfort, and future. With the right knowledge and expert guidance, you can navigate your healthcare with confidence and emerge healthier and empowered.